Marginalized communities concerned about changes to assisted-dying laws
Posted Jan 22, 2021 8:37 pm.
Advocates from Canada’s Black, Indigenous and disabled communities are concerned that proposed changes to medically assisted dying laws would let some of society’s most vulnerable people slip through the cracks.
“There is a history in this country of legislating this idea that disabled people don’t have the right to exist,” says Sarah Jama, an activist and organizer with the Disability Justice Network of Ontario. She also has cerebral palsy.
Canada’s current medically assisted dying law states that death must be reasonably foreseeable for someone to qualify. In 2019, Quebec’s disability community won a Superior Court ruling, stating that such criteria infringed on their rights. The federal government is now on deadline to update the laws by the end of February, including removing the clause that death must be imminent. If passed, someone with a disability or chronic pain would be able to access medically assisted death, known as MAID. The legislation is now before the Senate.
Jama says she is dismayed by the lack of Black and Indigenous voices in the MAID discussion which is before Parliament. She has asked to speak in front of the Senate. She believes Canada must first put proper supports in place for marginalized members of society before opening the laws around medically assisted death.
“How can you ensure that people who are struggling to survive – people who are living on poverty wages, who are on ODSP or social assistance, who cannot see another way out, will not access MAID because it’s the only other option?” she asks. “When you have a government that is allowing people the choice to die, without really funding the choice to live and survive in our country, it scares me.”
The government says the changes to the law are in line with the Quebec court decision, and allow people to make their own decisions about when it’s appropriate to die.
“There is already a lot of mistrust with the Canadian healthcare system so I think removing that consent …that’s just going to create a greater mistrust of the system between Indigenous peoples and the Canadian healthcare system.”
“It’s about autonomous decision making, respectful of life, respectful of death,” says Minister of Justice David Lametti. He adds that the proposed changes come after feedback from thousands of Canadians.
“The vast majority of Canadian’s support this and the vast majority of the medical community support this and we’ve determined it as a right under the Charter.”
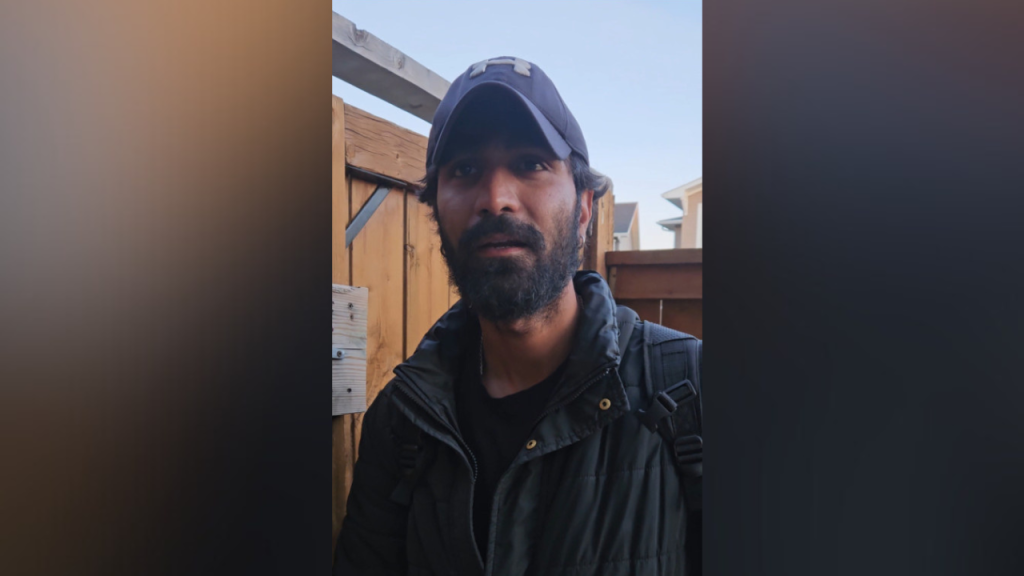
For a member of a racialized community that has historically been oppressed, the freedom to choose isn’t so clear, says River Holland-Valade, an Indigenous mental health outreach worker.
“In Indigenous communities, what a lot of our pain and suffering comes from is inadequate social supports,” they says. “Especially in the Indigenous community as a whole, let alone Indigenous disabled people. We’re talking about high poverty rates, overrepresentation in the justice system, overrepresentation of Indigenous children in child welfare, lower life expectancy, lower health status, higher rates of suicide, unemployment, it goes on and on.”
Holland-Valade also has been living with chronic pain and fibromyalgia for six years.
“If Bill C-7 had went into place a few years ago, it’s something I might have considered,” they say. “It’s hard to think about, I remember how hard it was, living day-to-day without having access to medications or treatment. If I had gotten diagnosed sooner I wouldn’t have even needed to consider something like MAID.”
For someone whose death isn’t reasonably foreseeable, under the proposed rules they would first have to complete a 90-day assessment period. But Holland-Valade points out it took four years for them to receive a diagnosis.
Even for doctors experienced in medically assisted death, the new rules open up concerns. Dr. Ed Weiss is a family doctor who has administered MAID to more than 100 patients since its early days of legality in Canada.
“When MAID is restricted to people with a specific diagnosis that is expected to cause their death, it seems morally easier in a sense. It does get more complicated when we’re talking about chronic pain syndromes,” he says. “We’re going to have to have some really robust assessment processes to really suss out, for the people who don’t have a reasonably foreseeable natural death – have they really tried everything, are they informed about all their options?”
He points out that right now MAID is mostly administered by doctors and nurse practitioners as just a small part of their practices. He suggests that it should be put into the hands of dedicated specialists who can ensure a patient is fully informed and empowered.
Jama also points out that for racialized people, the existing bias in the medical system may influence their treatment, and decision to choose MAID.
“You don’t actually have to get training on ableism, you don’t have to get training on this history of disabled people in Canada, you don’t have to get real training on anti-racism to become a doctor,” she notes.
Another proposed change to the laws would remove the rule that someone must be able to consent right up to the moment they’re about to die. Dr. Weiss says that’s a relief for terminally ill patients who worry they’ll lose their capacity to consent, and be trapped in a vegetative state. But disability advocates say it hasn’t been considered from the perspective of communities that have been historically traumatized by the medical system.
“There is already a lot of mistrust with the Canadian healthcare system,” says Hollande-Valade “So I think removing that consent […] that’s just going to create a greater mistrust of the system between Indigenous peoples and the Canadian healthcare system.”